You expect sniffles, sneezes, and stuffiness when you have a cold. Sometimes, though, there’s little respite and symptoms linger far longer than you anticipated. In fact, they can last for months or even years. This is called chronic rhinitis. If you’ve been struggling with nasal symptoms and haven’t found answers, this article will walk you through all of the (many) causes of chronic rhinitis, important functional testing, and the lifestyle and medical interventions that make up an effective treatment regimen.
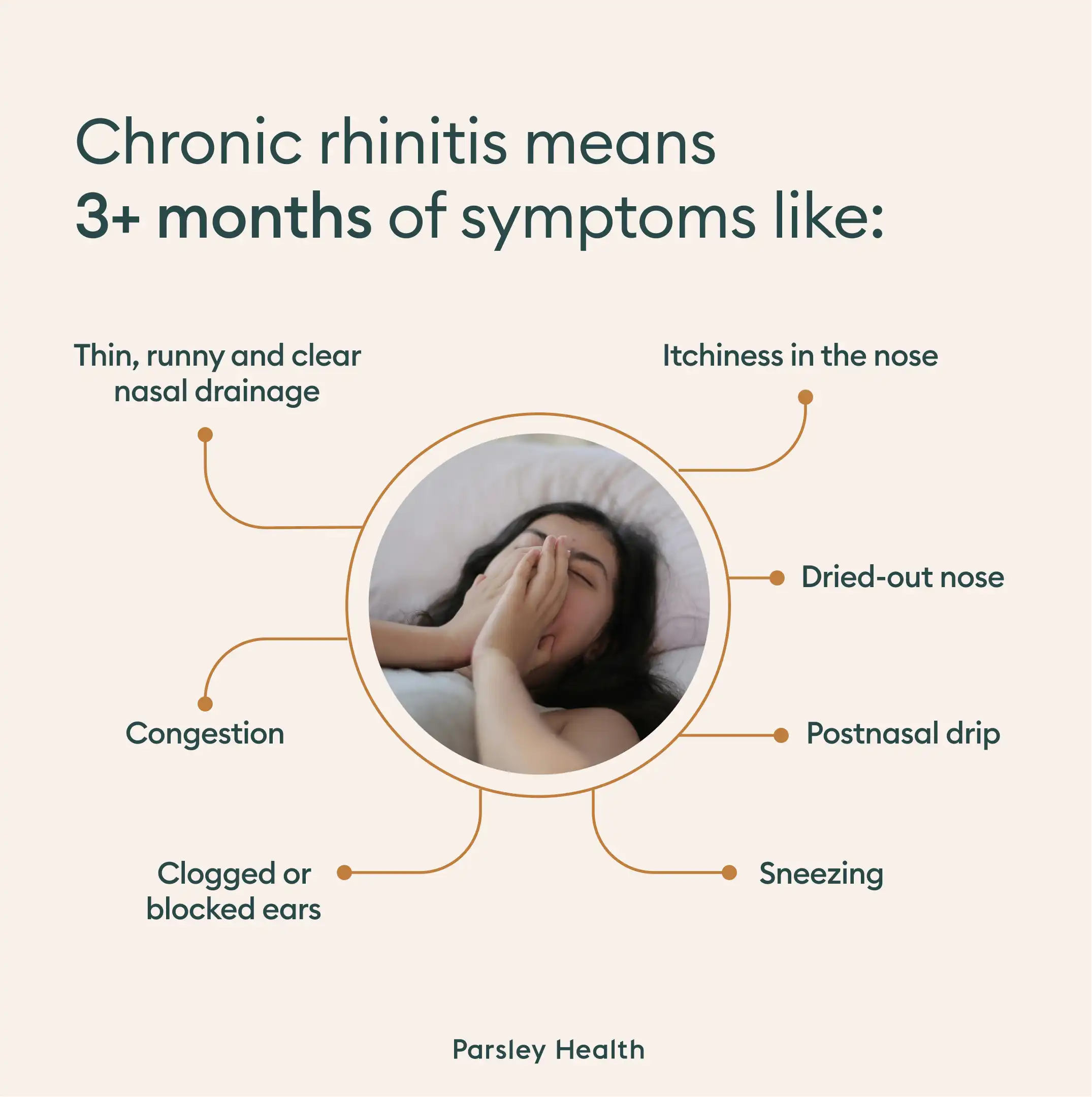
Annoying nose itchiness? Constant postnasal drip causing you to clear your throat all the time? Sneezing that makes people ask "how are you still sick?" Sounds like it could be chronic rhinitis, a condition featuring symptoms like congestion and a runny nose that lingers for way too long. It can be extremely frustrating to try to treat chronic rhinitis, because there are so many causes. Some treatments may address your symptoms a little bit, but for full control, you’ll need comprehensive testing so you and your doctor can take a root-cause approach and develop targeted treatments. Here’s where to start.
What is chronic rhinitis?
First, let’s talk about rhinitis. “Rhinitis is inflammation of the nose,” says otolaryngologist Tonia Farmer, MD (aka Dr. Nose Best). There are two types of rhinitis:
- Allergic (caused by things like seasonal allergies)
- Nonallergic (caused by things like a viral infection)
If you’re stuffed up with a cold for a week (or more), it can feel like a clogged-up nose will never go away. But, once your body clears the virus from its system and inflammation subsides, rhinitis should ease up, too. This is an example of acute rhinitis.
Chronic rhinitis, however, comes in when symptoms (see below) are present for more than three months, says Jessica Lee, MD, a double board-certified physician in otolaryngology and lifestyle medicine in Charleston, SC.