Frequent heartburn isn’t just uncomfortable, it can be a sign of gastroesophageal reflux disease (GERD), a chronic condition in which stomach acid regularly flows back into the esophagus. Over time, untreated GERD can irritate the esophageal lining and increase the risk of complications, which is why many people wonder: can GERD be cured permanently?
The answer is nuanced. While GERD doesn’t always have a one-size-fits-all “cure,” many people are able to achieve long-term relief by addressing the underlying causes of their reflux. Diet, eating habits, stress, gut health, and certain medical conditions can all play a role. Understanding how these factors interact is key to reducing symptoms and preventing them from returning.
In this guide, we’ll break down what causes GERD, evidence-based strategies that may help improve symptoms, and when medical treatment is appropriate. We’ll also explore how a personalized, root-cause approach, often used in functional medicine, can help some people manage GERD more effectively over time.
Not sure what your symptoms are really telling you?
The Parsley Symptom Index helps connect the dots across your whole body so you can understand patterns, not just isolated symptoms.
What Is GERD or Gastroesophageal Reflux Disease?
GERD stands for gastroesophageal reflux disease. We can better understand it by differentiating acid reflux from GERD. These are similar but differ in a key way:
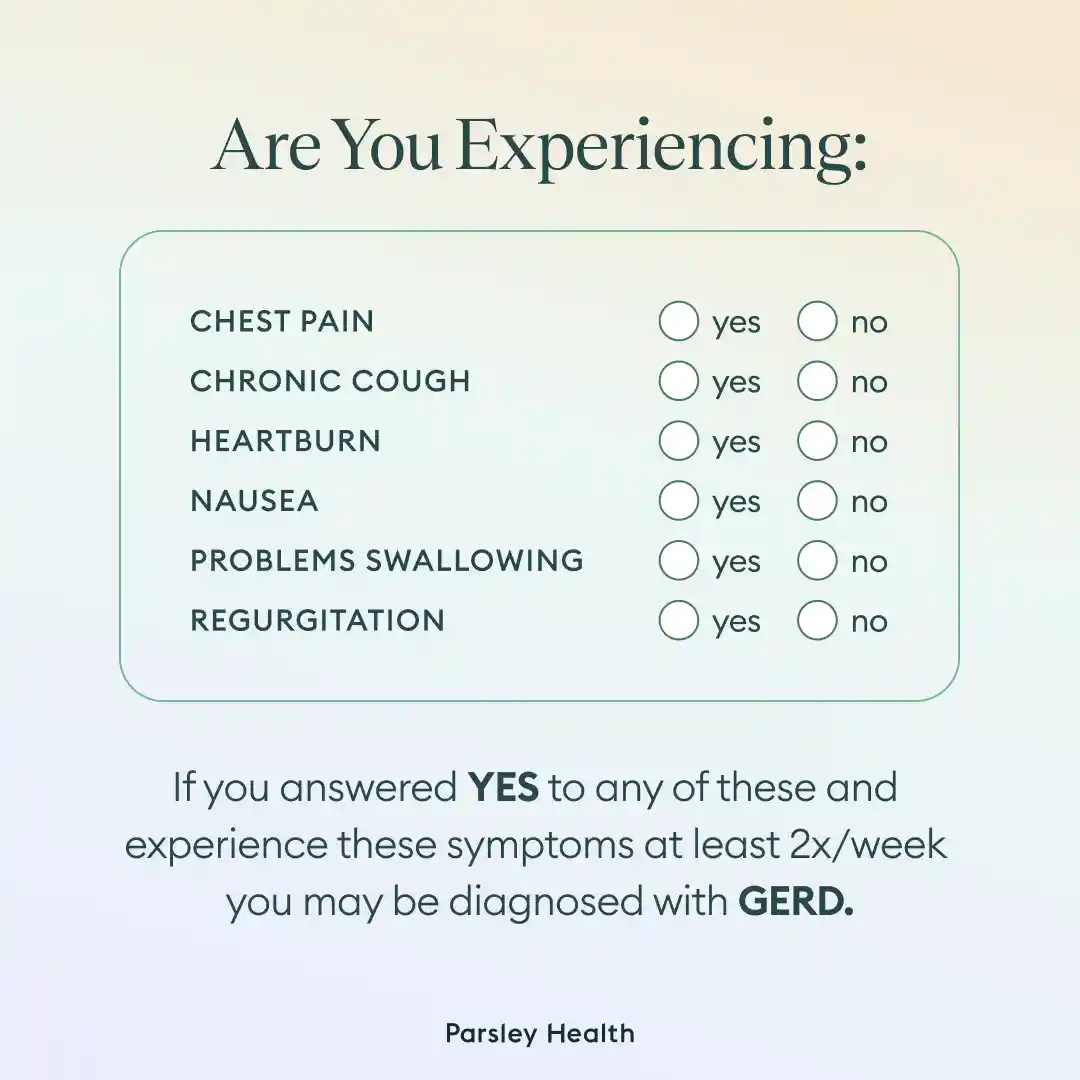
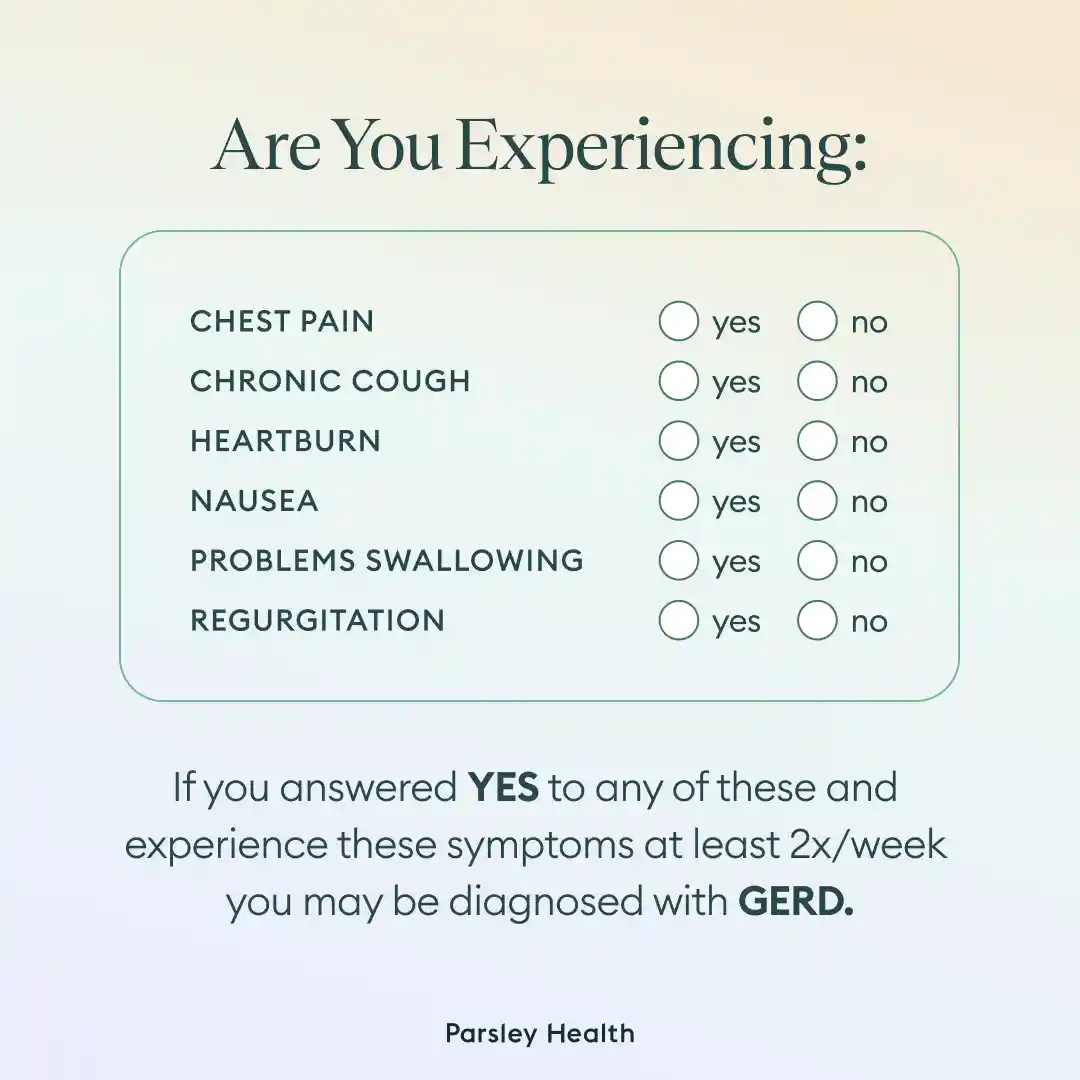
- Acid reflux is when the contents of your stomach bubble back up into your esophagus, causing symptoms like:
- Chest pain
- Chronic cough
- Heartburn
- Nausea
- Problems swallowing
- Regurgitation (which can cause a sour or bitter taste in your mouth)
Although reflux is not normal, it is something that can happen on occasion after you’ve eaten a big meal or one of your trigger foods.
- GERD is a chronic condition where you experience acid reflux or the above symptoms consistently. You may be diagnosed with GERD if you have acid reflux at least twice a week for several weeks. Risk factors for GERD include being overweight or obese, being pregnant, taking certain medicines, and smoking.
Other conditions can feel similar to GERD, such as indigestion. To differentiate GERD from other conditions, you'll need a complete evaluation of your gut from a functional medicine provider. They will look at the health of your gut microbiome, including screening for small intestinal bacterial overgrowth (SIBO) and stool testing to look for infections like Helicobacter pylori (H. pylori).
The results of these tests will lead to a protocol for gut healing that focuses on shifting the microbiome or treating abnormalities that are found. This approach alone can cure GERD permanently.
Lifestyle changes to manage and potentially cure GERD
When it comes to gastroesophageal reflux disease treatments, you’ll be most successful by taking a two-pronged approach. “I like to attack GERD in a multifaceted way,” says Supira Rao, MD, a board-certified physician specializing in gastroenterology and lifestyle medicine. “Medication can definitely help, but lifestyle modification can make a huge difference,” she says.
The lifestyle changes needed will be different for everyone. So, while we’ve included a general list below, know that you may not need to incorporate all of them. A functional medicine provider can help you identify what you need and create a customized plan.
Dietary adjustments for GERD
There are many changes you can make to your eating habits to help decrease GERD symptoms.
- Limit or avoid trigger foods. Specific trigger foods differ for everyone, but certain foods are known to weaken the lower esophageal sphincter (the muscle at the bottom of the esophagus that stops stomach contents from coming up) or irritate the lining of the esophagus, says Erika Jacobson, M.S., RD, a functional gut health dietitian. These foods that should be avoided for most include:
- Alcohol
- Carbonated beverages
- Chocolate
- Citrus
- Coffee
- Fried and greasy foods
- Garlic
- High-sugar foods
- Onion
- Peppermint/spearmint
- Spicy foods
- Tomatoes and tomato sauce
- Avoid large meals and overeating. Aim to feel 80% full, Dr. Rao recommends.
- Slow your eating speed and chew your food thoroughly. “I recommend chewing food until it’s an applesauce consistency,” says Jacobson. “This helps optimize digestion to properly break down and absorb food,” she adds.
- Eat a high-fiber diet. Eating foods that contain fiber—fruits, vegetables, whole grains, legumes, nuts and seeds— can improve your lower esophageal sphincter pressure and reduce reflux and heartburn, according to a small study in the World Journal of Gastroenterology. These foods are also more filling and can naturally help prevent overeating. Eating more of these foods can help crowd out ultra-processed foods in your diet that are more likely to trigger symptoms.
- Walk after eating. This promotes gut motility and digestion. (It prevents food from just hanging around in your stomach, Dr. Rao says.)
Weight management
Obesity and being overweight are risk factors for GERD. “If you have increased weight, especially around the abdominal area, a five to 10 percent decrease in weight can improve symptoms,” says Dr. Rao. One study on adults with obesity found that 65 percent of those who lost a modest amount of weight had a complete resolution of their GERD symptoms.
Weight management isn’t a simple solution. Working with a provider who is knowledgeable in diet, lifestyle medicine, or obesity medicine—or connecting with a registered dietitian who specializes in weight loss—can help you draw up a plan to reach a healthy-for-you weight.
Sleep and positioning tips
How you sleep affects GERD symptoms since lying down makes it easier for your stomach contents to come back up (they don’t need to fight gravity!). Here are a couple things you can do to mitigate this:
- Wait three hours after eating before lying down or going to bed. “When your stomach is full of food, it’s more likely to reflux back up into your esophagus,” says Dr. Rao.
- Elevate the head of your bed, which helps keep acid in your stomach. You can do this by using specialized pillows or mattress wedges, or even sliding books under the legs at the head of your bed.
Stress reduction
Stress can be a doozy for eating habits, causing you to comfort-eat foods you otherwise might not (like fried, greasy meals). “Stress affects your body’s ability to properly digest and break down foods. As a result, you can get poor digestion and gas, as well as low or excess stomach acid,” says Jacobson. Think about what actually decreases your stress, and actively plan ways to incorporate these habits into your life. You can try breathwork, journaling, walking, meditation, or spending quality time with pets and people you love.
Personalized dietary approaches
We all have our own dietary triggers that make acid reflux more likely. Learn about yours and modify your behavior to limit or avoid them completely as necessary. Jacobson recommends keeping a food journal to help you better identify triggers. If you’re not sure, you can try a short-term elimination diet at home where you eliminate certain trigger foods and reintroduce them one at a time, watching for symptoms. The most successful way to try an elimination diet is under the supervision of a registered dietitian.
Some providers also use food sensitivity testing to identify potential trigger foods and tailor your diet to your body’s specific needs.
Healing stories from our members
Medical treatments for GERD
Medications may be an important component of GERD treatment for some patients, but not every patient will need medication. If medications are recommended, they must be paired with lifestyle modifications. “Medications have their place, but it’s not helpful if you don’t take them alongside lifestyle changes,” says Dr. Rao.
Over-the-counter medications
You may opt to take antacids for occasional, mild heartburn relief. Taking one of these medications on occasion does not necessarily mean you have GERD, but needing them on a daily basis is a problem.
For more severe symptoms, you might take stronger medications for GERD, such as: H2 blockers like famotidine (Pepcid), a proton pump inhibitor (PPI) like omeprazole (Prilosec), or esomeprazole (Nexium). These can be purchased over the counter, and they work by reducing stomach acid.
Prescription medications
Products like PPIs are also available by prescription, and contain the same medications as their OTC form. Although both OTC and Rx versions generally have the same dosage, they’re used in slightly different ways. OTC products are indicated to address symptoms (heartburn), while prescription products are indicated to treat a medical condition (GERD). If you’re not sure if you should take an OTC or Rx medication for your symptoms, talk to your provider.
Innovative non-surgical interventions
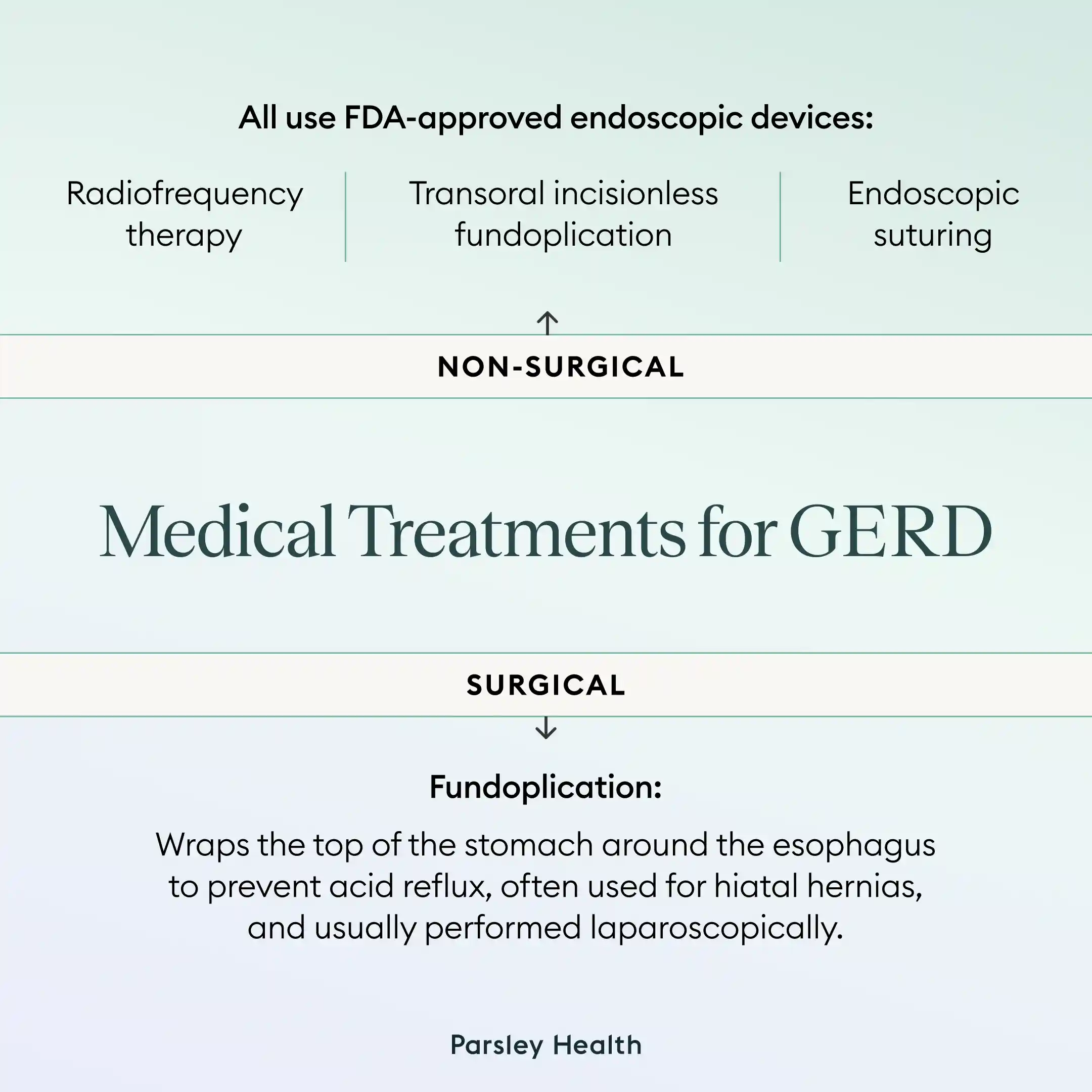
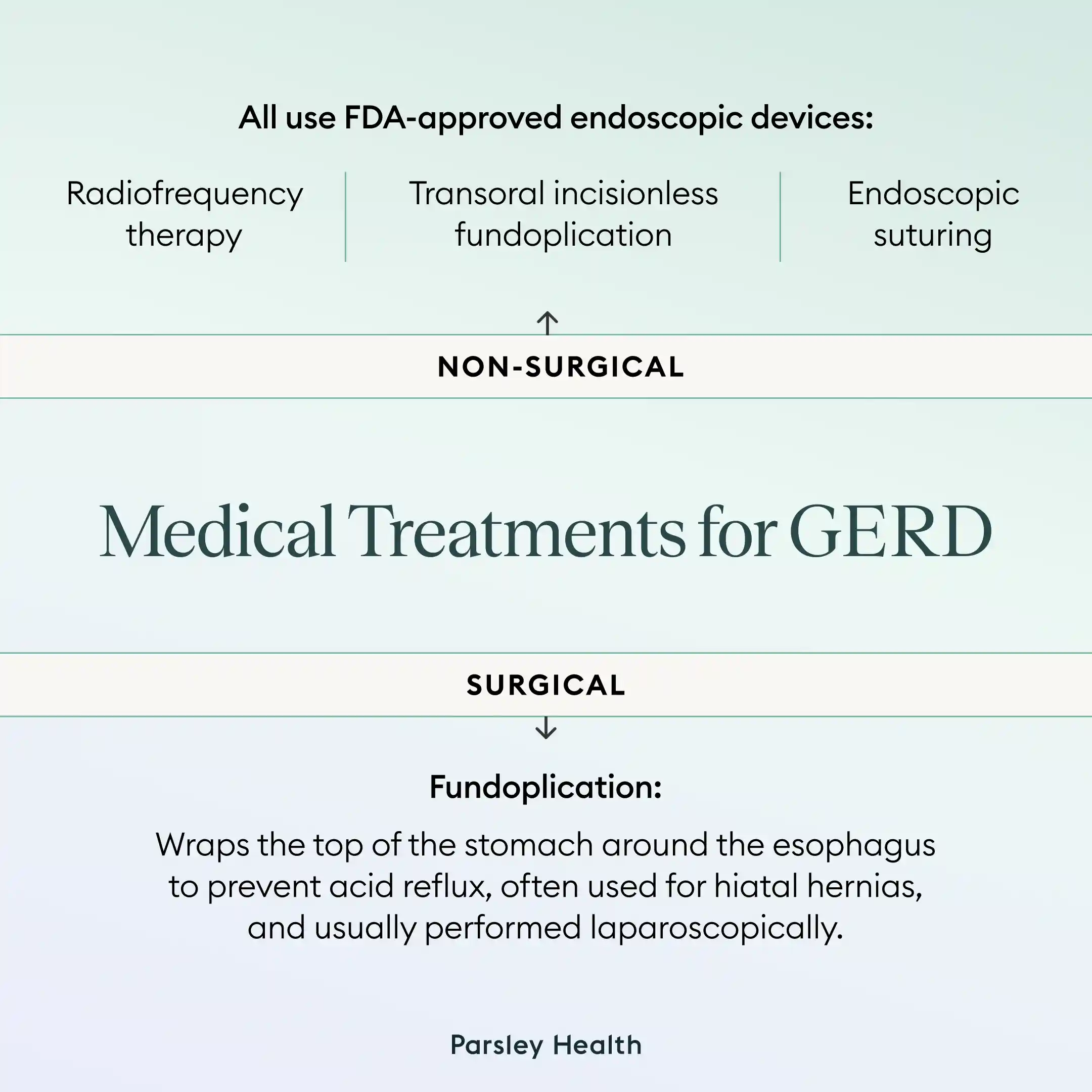
Non-surgical options include FDA-approved endoscopic devices to treat GERD:
- Radiofrequency therapy (which uses low-frequency energy to help strengthen the lower esophageal sphincter to stop reflux)
- Transoral Incisionless Fundoplication (a procedure that reconstructs the sphincter)
- Endoscopic suturing (a procedure that uses sutures to reinforce and tighten the sphincter)
These may be appropriate to address anatomical problems that are contributing to persistent GERD symptoms. Non-surgical interventions also have fewer side effects, like gas and bloating compared to surgical procedures. Whether you’d benefit from one of these procedures—and which one is right for you—depends on various factors, such as your symptoms, health history, and any anatomical problems. Talk to your healthcare provider about the best option for you.
Surgical options
Your provider may recommend surgery if you have specific underlying problems contributing to your GERD, or if lifestyle and medication therapies did not work to control your symptoms. One surgical procedure they may consider for you is called fundoplication, which can directly treat GERD. It can be used to fix a hiatal hernia, when part of the stomach pushes up through an opening in the diaphragm and allows acids to more easily come back up into the esophagus.
This surgery involves wrapping the top portion of your stomach around your esophagus, which creates more pressure to keep your stomach contents down where they should be. It’s something that can be done laparoscopically, which means it’s a minimally invasive procedure involving small incisions.
Natural and alternative remedies
Your functional medicine provider may also recommend certain herbal supplements—along with stress reduction and getting quality sleep—to relieve symptoms of GERD. What’s right for you will depend on your symptoms, any underlying causes of your GERD, and your personal health. Jacobson often recommends the following.
- Ginger: This rhizome can be helpful in reflux that’s triggered by slow gastric emptying (the movement of food out of the stomach). It can be taken as a supplement, used in cooking (as a powder), or sipped as a tea.
- Bitters: “These help trigger the release of enzymes that promote stomach acid and bile production, supporting overall digestion and reflux symptoms,” says Jacobson. Take bitters about 10 minutes before eating. Place these directly on your tongue to activate the salivary process and get the digestive system ready for the meal.
- Mucilaginous herbs: DGL (deglycyrrhizinated licorice), marshmallow root, and slippery elm are just a few of these herbs that are available in powders, teas, and supplement form to soothe inflamed tissue.
Any time you are taking supplements, make sure to purchase those that are third-party certified, which ensures safety and accurate labeling of the product.
Parsley Health offers physician-led functional medicine care, advanced lab programs, and flexible ways to get started, all designed to help you feel better over time.
When to seek medical advice for GERD symptoms or acid reflux
It’s a good idea to try to avoid acid reflux episodes whether you have GERD or not. (You can do this, for example, by avoiding overeating or staying away from your personal trigger foods.) Acid reflux becomes a chronic problem when:
- You experience symptoms multiple times per week, week after week.
- You’re taking an over-the-counter medication every day or most days for acid reflux or indigestion symptoms.
- You wake up in the morning with an acid taste in your mouth.
- You have difficulty swallowing.
In the above instances, Dr. Rao recommends seeing a provider.
GERD is not a benign condition. Having constant acid exposure to your esophagus can cause inflammation and ulceration to your esophageal tissues. Over time, this can also make you more prone to something called Barrett’s esophagus, says Dr. Rao. “This is when the cells in the lining of the esophagus start to change. It’s the first step in many toward esophageal cancer,” she explains. Besides, GERD causes major discomfort—that alone is reason enough to seek care.
Talk to your provider about further evaluation, which may include an upper endoscopy to look at the tissues of the esophagus.
Can GERD be cured permanently?
Yes, in many instances GERD can be cured permanently, but a comprehensive testing and treatment approach is needed. “We want to do a root-cause analysis to determine what is causing your GERD,” says Jacobson. There are so many potential contributors to the condition, she says, including:
- Excess acid production
- Slow motility
- Hiatal hernia
- Reduced lower esophageal sphincter pressure
- Low stomach acid
- Poor digestion
- Dysbiosis (imbalance in gut bacteria)
- SIBO
Treating and managing symptoms is important, but they won’t disappear altogether if you don’t address them and their underlying causes. Treating these and adhering to recommended lifestyle changes is what will help you cure GERD for good.
Tips for long-term GERD prevention
You’ll want to maintain your new habits to prevent GERD from coming back in the future, and that includes dietary changes, exercise habits, and stress reduction strategies. Remaining consistent with these healthy habits will help you feel good long-term.
If symptoms re-emerge, don’t hesitate to reach back out to your provider. GERD symptoms can come back due to changes in your eating habits, but they may also be an indicator of additional problems or conditions to address.
Frequently Asked Questions about GERD
What is the fastest way to cure GERD?
Lifestyle changes will make a big difference in your GERD symptoms. So eat slowly, chew your food thoroughly, focus on eating smaller meals, and avoid eating at least three hours before lying down for bed. Medication, such as over-the-counter H2 blockers or PPIs, may also relieve symptoms, but there’s no fast fix. It’s important to get to the root cause of your GERD and focus on treating that.
Is GERD curable permanently?
Yes, GERD can be cured permanently in many patients. GERD is caused by a variety of conditions, including SIBO, certain types of hernias, high or low stomach acid production, digestive problems, and more. Identifying and treating the underlying can help heal the gut. Changes in eating and other lifestyle habits can also relieve symptoms.
How do you flush acid out of your stomach?
If your provider has told you that you have excess stomach production, some things that can help regulate it include taking H2 blockers or PPIs to reduce stomach acid production. Antacids can also help neutralize stomach acid.
Can I heal GERD on my own?
You can start treating GERD at home by making lifestyle adjustments like eating smaller meals, slowing down eating speed, and chewing food thoroughly. Taking walks after meals to encourage healthy digestion, incorporating stress relieving strategies into your life, and sleeping with your head elevated can address symptoms in an impactful way.
For the best chance at curing GERD, a multiprong approach that involves deep-dive testing can help you get to the root cause and resolve it. You can go ahead and start with some of the smart digestive-supporting strategies outlined above, but you’ll get a lot of benefit out of connecting with a clinician, like one at Parsley Health, who can help you put together a comprehensive gut health plan that helps you make changes that work with your lifestyle. You can feel good after eating again.
Key Takeaways
- GERD can be healed naturally once you identify and treat the root cause(s). This requires a comprehensive testing approach to uncover the source of your digestive dysfunction.
- Following an individualized gut healing protocol can bring long-term relief. Lifestyle modifications are just as important as medications when it comes to relieving symptoms of GERD.
- Surgical procedures may be recommended if traditional treatment for GERD is not effective for you or in certain underlying medical conditions.
- For long-term symptom relief or curing GERD requires adhering to the lifestyle changes that work for you. Because triggers are individualized, it’s beneficial to have a customized plan in place, and working with a knowledgeable functional medicine doctor and nutrition coach can help make this happen.