Allergies can sometimes cause fatigue because your immune system is trying to protect you from a perceived threat. The resulting inflammation can tank your energy level. Allergies can also disrupt your sleep because the release of the chemical histamine causes wakefulness. Allergy symptoms can keep you tossing and turning, as well, leading to next-day tiredness. Some older allergy medications can also make you feel drowsy. Newer meds, lifestyle changes, and other strategies can help you cope.
I can personally and scientifically confirm that the answer to your question “Can allergies cause fatigue?” is a resounding YES.
I write this while currently sniffling, sneezing at my desk, and wishing I could lounge in bed with a good book and a box of tissues. But, hey, I’m here for you and ready to dive deeply into how and why allergies can cause us to feel tired, rundown, and wishing we could hibernate. Plus, we’ll explore how to combat allergy-related fatigue and feel more energetic, even in the face of triggers.
Understanding allergy-related fatigue
Think of your immune system as the mama bear of your body. If it senses a threat coming at you, it’s going to launch an all-out attack to try to protect you. In this case, the threat could be anything from pollen to ragweed or from dust mites to animal dander.
At the first sign of one of these allergens, your immune system produces antibodies called immunoglobulin E (IgE). These antibodies tell specific cells (called mast cells) to release a chemical called histamine. Once your cells release histamine, the chemical binds to histamine receptors (we have four different types), resulting in an allergic reaction. Typically, with environmental allergies, histamine is binding to H1 receptors, leading to symptoms like sneezing, coughing, itchy and watery eyes and nose, and inflamed or itchy skin.
Whether your mama bear immune system jumps into action will depend on whether you have a specific allergy. For example, I am allergic to cat dander, so I have cat-dander-specific IgE antibodies. If I pet a cat and then touch my face, I’ll have a major reaction. My husband is not allergic to cats, so he doesn’t have cat-dander-specific IgE antibodies and can let cats crawl all over him without concern. (Can you sense my jealousy?)
So what does this all have to do with fatigue? An allergic reaction involves inflammatory processes that can leave you feeling tanked. “The inflammatory response from the immune system takes a significant amount of energy, which also contributes to the excess fatigue and brain fog many individuals report,” says Trista Best, RD, a registered dietitian at The Candida Diet.
Histamine is closely tied to your sleep-wake cycles, as well. Researchers have known for decades that our histamine levels are highest in the early morning and that histamine causes wakefulness. But, for this reason, histamine can also impact your ability to fall or stay asleep, leading to a lack of quality pillow time. Allergy symptoms can also keep you wide awake and cuddling with the tissue box.
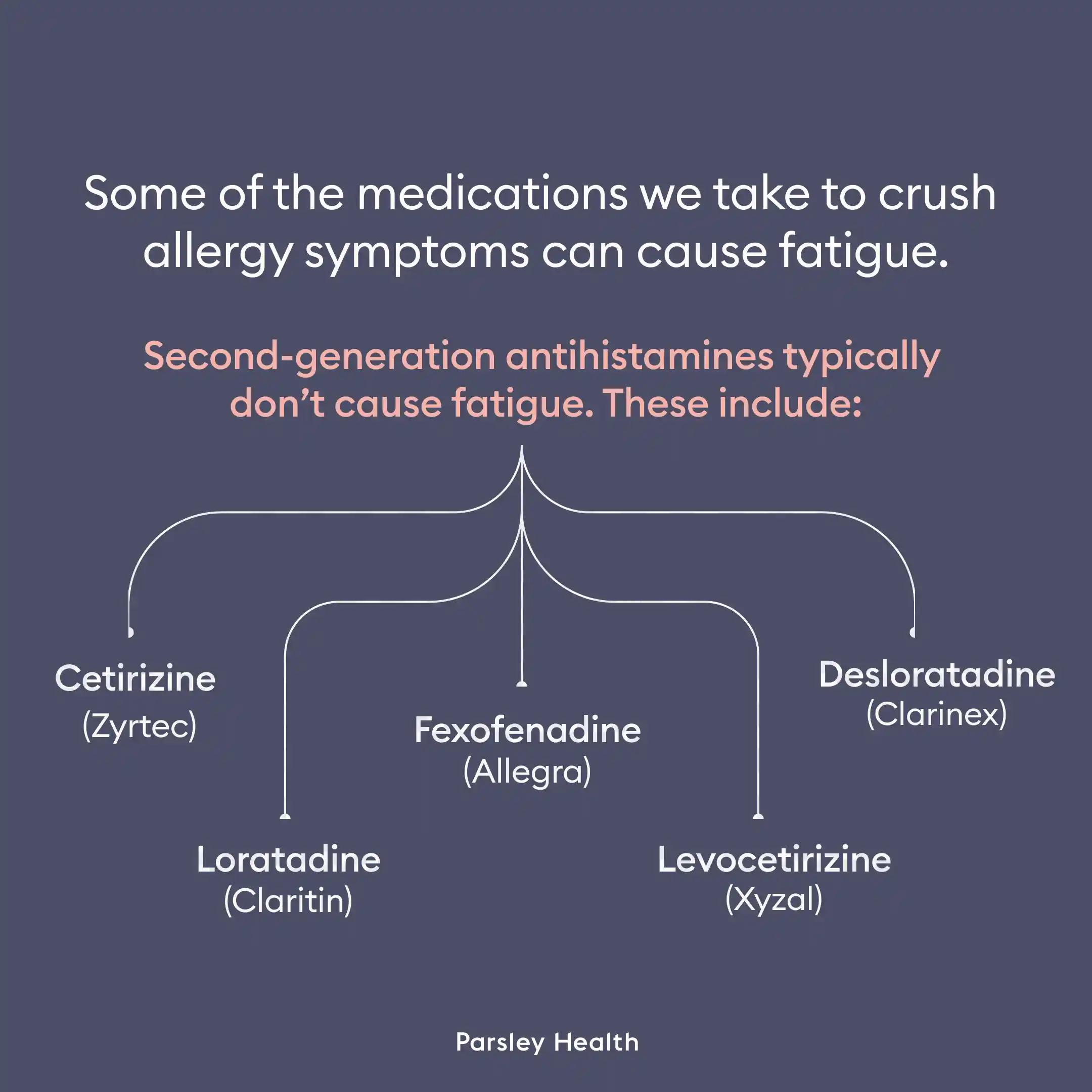
Complicating matters is that some of the prescription and over-the-counter medications we take to crush allergy symptoms can cause fatigue. These are called antihistamines because they block certain histamine receptors. Older antihistamines (known as first-generation antihistamines) can especially make us feel the need for a nap. Doxylamine, a common first-generation antihistamine, can be found on the ingredient list for meds like NyQuil, designed to help us sleep better when we have a cold. But second-generation antihistamines typically don’t cause fatigue.
First-generation antihistamines
- Diphenhydramine (Benadryl)
- Doxylamine (Unisom)
- Chlorpheniramine (Chlor-Trimeton)
- Hydroxyzine (Vistaril)
Second generation antihistamines
- Cetirizine (Zyrtec)
- Loratadine (Claritin)
- Fexofenadine (Allegra)
- Desloratadine (Clarinex)
- Levocetirizine (Xyzal)