What does “recovery” from COVID-19 look like? The fact is, we still don’t really know. As with many other things that are unknown about the disease caused by the novel coronavirus, the lingering effects of the illness—if any—are largely unknown. Still, whether you’ve had a mild case of COVID-19 or a more severe illness, there are things you can do to support your body after if it’s been through a difficult infection.
When your body goes through any type of illness, particularly something as trying as COVID-19, it ultimately comes away weak and rundown, even after your body has successfully cleared the virus. That’s because infections cause an inflammatory response in the body. Cytokines, small proteins secreted by cells in the immune system, and other inflammatory molecules become elevated to fight the infection. This increased inflammation can lead to post-viral fatigue, lethargy, difficulty concentrating, and sleep changes. In the case of a respiratory illness like COVID-19, there is likely ongoing lung inflammation, and potential damage, that needs to be addressed as well.
At Parsley Health, our doctors and health coaches have been working closely with our members who are recovering from COVID-19. While each case is different, there are a few recommendations we’re advising our members with COVID-19 to implement post-infection.
1. Eat an anti-inflammatory, low carbohydrate diet.
Even after your immune system has cleared the virus it may take some time for heightened inflammation to normalize. This is why sticking to an anti-inflammatory diet is particularly important. An anti-inflammatory diet emphasizes specific vitamins, minerals, and nutrients found in whole foods that play a direct role in combating the internal inflammatory response. Similarly, limiting the intake of highly processed foods with pro-inflammatory properties will minimize any unnecessary additional inflammation.
These anti-inflammatory nutrients can be found in fruits, vegetables, well-sourced animal and plant based proteins, nuts, seeds, and whole grains. Specifically, omega-3 fatty acids found in wild caught salmon, sardines, anchovies, flax seeds, chia seeds, and walnuts are highly anti-inflammatory—helping to switch off inflammatory pathways in the body. Antioxidants such as vitamin C, vitamin E, and beta carotene found in broccoli, bell peppers, citrus fruits, kiwis, almonds, sunflower seeds, avocados, sweet potatoes, and carrots protect your cells from the effects of free radicals therefore, counteracting oxidative stress and reducing inflammation.
For those that are recovering from severe lung infection, it’s worth noting that certain macronutrients may be more aggravating than others. For example, carbohydrates use more oxygen and produce more carbon dioxide when digested, whereas fats produce less. In other words, what you eat can directly impact the workload of your lungs. While research regarding COVID-19 and nutrition is yet to be investigated, in other lung conditions such as chronic obstructive pulmonary disease (COPD), eating a diet with fewer carbohydrates and more healthy fats positively affects breathing. Through the lens of an anti-inflammatory diet, this means focusing on the fats contained in nuts, seeds, avocados, and olives and consuming fewer carbohydrates from starches like pasta, breads, and grains.
2. Re-regulate your sleep-wake cycle.
You might be excited that you’re finally well enough to stay up late and binge Tiger King on Netflix, but getting in 8 or more hours of quality sleep—and at normal hours—is more important now than ever. When you sleep, your brain releases hormones that encourage tissue repair. During certain hours, like between 2AM and 4AM, your body’s rate of cellular turnover while sleeping triples—literally accelerating the body’s much needed recovery.
It’s likely that the irregular sleep patterns you had while acutely ill have thrown your body off its natural circadian rhythm. To help get back into an optimal routine, work on getting to bed between 8PM and 12AM nightly, ideally around 10PM, and sleeping for at least 7 hours as recommended by the National Sleep Foundation. Research shows that exposure to bright light in the morning by getting outdoors to take a walk or sitting near a sunny window can help to recalibrate the body’s internal clock. This can make it easier to fall asleep and reduce the number of disturbances you experience at night.
Likewise, it’s important to avoid bright light later in the day or at night, so refrain from using your phone, TV, or computer 60 minutes before bedtime. Set up a wind down routine by dimming the lights, burning candles, reading a book, or taking a hot shower to calm your mind and your body. Engaging in these calming activities before bed will stimulate the secretion of melatonin and prepare you for the restorative rest you need while continuing to fully recover.
3. Get back to movement.
After just a few weeks of little or no exercise, your body begins to weaken and atrophy. It’s nothing to panic about, but exercising after you beat an illness helps your body regain strength by encouraging your joints, muscles, and organs to become accustomed to a higher level of activity. Outside of increased physical strength, exercise can help to lower blood pressure, increase levels of mood-enhancing compounds called endorphins, and allow for greater amounts of oxygen to circulate throughout your bloodstream—a benefit of the utmost importance when recovering from a respiratory illness that likely impaired your blood oxygen levels.
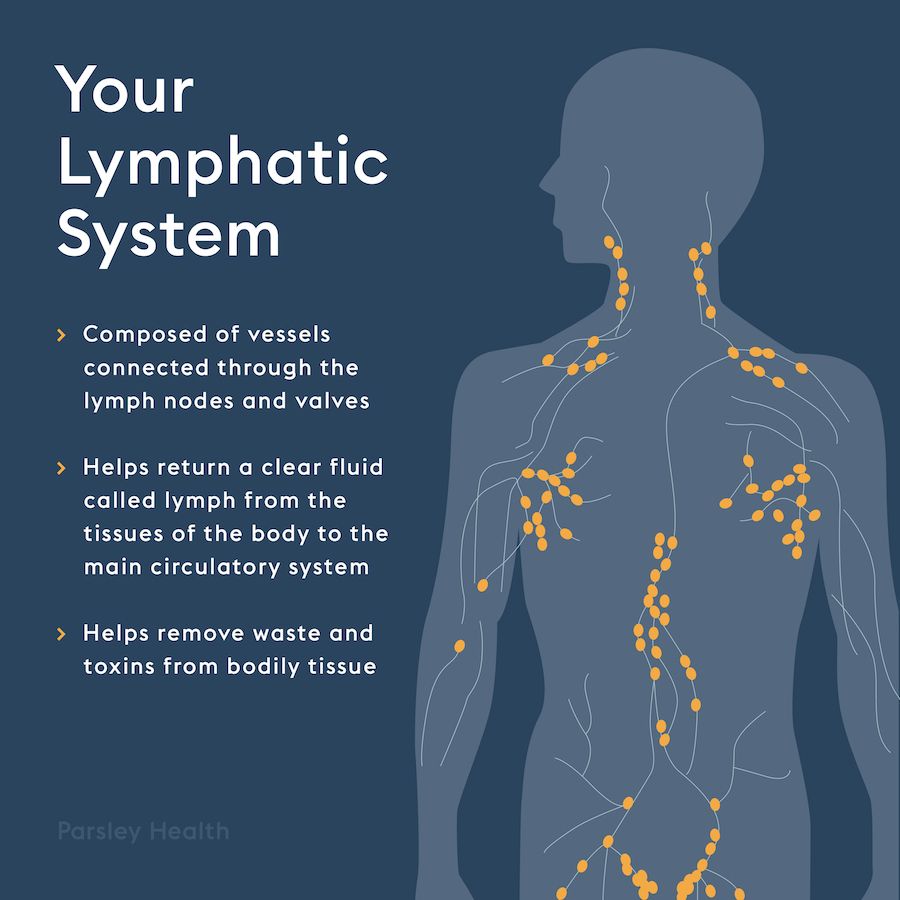
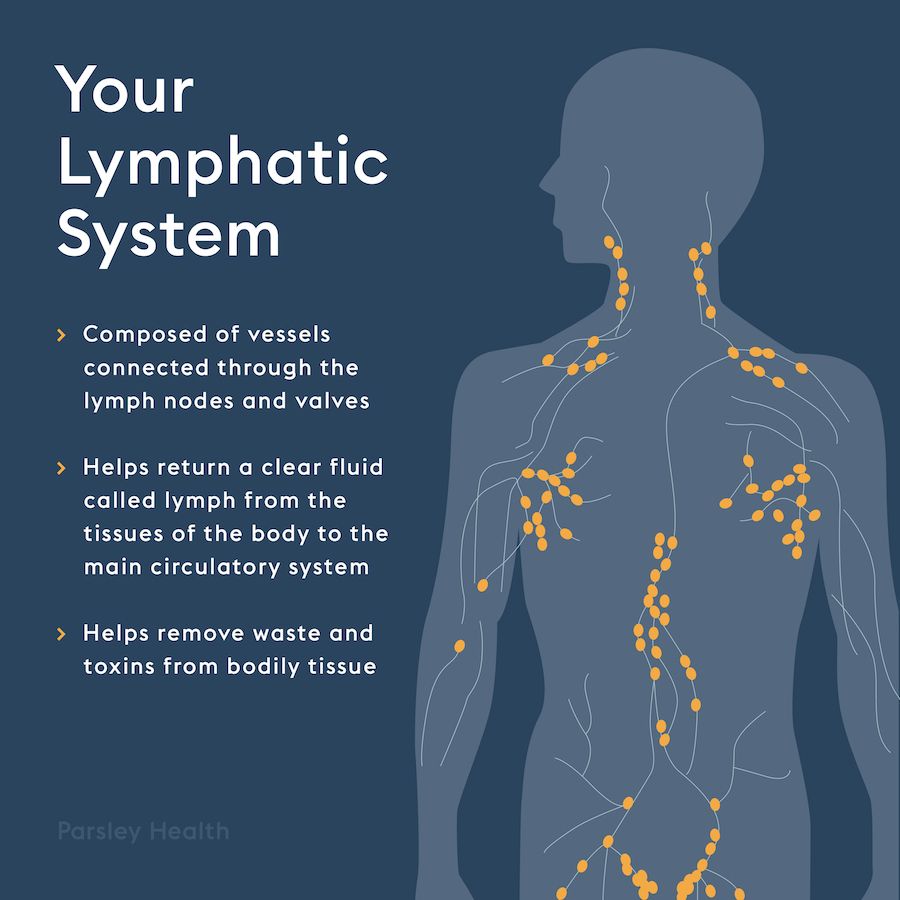
When getting back into exercise, it’s ideal to pick movement that supports lymphatic flow, the fluid that contains infection-fighting white blood cells, throughout the body. Supporting the lymphatic system in recovery accelerates the process of ridding the body of any built up toxins that accumulated while sick and sedentary. Exercise such as rebounding on a trampoline, practicing yoga, or even jumping rope or doing jumping jacks can help to kick the lymphatic system into high gear.
While movement is important to incorporate in your recovery regimen, refrain from reverting back into your old exercise routine too quickly. We recommend starting with about 20 minutes per day of gentle movement including some of the above exercises in addition to regular walking, stretching, jogging, or biking as tolerated.
4. Develop a deep breathing practice.
In severe cases of COVID-19, it’s possible that lung damage can occur as a result of pneumonia, acute respiratory distress syndrome (ARDS), or sepsis. In those instances, patients may need continued treatment and therapy as directed by a physician. For ways to support lung recovery at home, studies show deep breathing can help by clearing mucus from the lungs, opening up the air passages, boosting circulation and oxygen supply, and preventing the risk of recurrent lung complications such as pneumonia. Deep breathing also greatly improves lymphatic flow and drainage.
To start your deep breathing practice, get in a comfortable position, place your hands on your stomach, and inhale through your nose until you feel your lungs completely fill with air—feeling the expansion of your chest and belly against your hand. Slowly blow air out in one long exhale through pursed lips and feel your stomach fully sink inward. Repeat this breathing series for five full cycles. When complete, end with a short huffing series. Huffing is a short sharp pant—like exhaling onto a mirror or window to create mist. Inhale for 3 second then huff out three times. Repeat this maneuver two more times and then follow with one strong cough to clear mucus from the larger airways.
Ideally, try to complete this routine two to three times daily for a minimum of 3-4 weeks while recovering.
As an added bonus, deep breathing also stimulates the parasympathetic nervous system, which promotes a state of calmness—reducing anxiety and effectively lowering stress-related markers of inflammation that may be elevated post-infection.
5. Support your immune health.
After your immune system has put up a trying fight combatting the novel coronavirus, specific supplements, in addition to your nutritious anti-inflammatory diet, may help to support your immune health.
At Parsley Health, our doctors work with our members to assess the ideal supplement regimen based on their medical history and treatment plan, but common immune supportive supplements post-infection may include a high quality multivitamin, omega-3 fatty acids, broad-spectrum probiotics, vitamin C, and zinc. Other supplements such as quercetin, melatonin, and fibrinolytic enzymes may also be recommended for those that suffered more severe illness.
How long does it take to recover from coronavirus?
As with many things regarding the novel coronavirus, the exact timeframe in which it takes to recover from the illness—including how long someone remains contagious—is not fully known. It will take more time and data to answer these questions. For now, we encourage members to follow CDC guidelines and to continue to work closely with their doctors to determine what is best for each individual case.
Overall, the goal in recovery is to support your body with the nourishment it needs—both mentally and physically—to thrive post-infection. Focusing on getting your body back into balance with proper nutrition, adequate sleep, increased physical activity, deep breathing, and limited stress are the foundational elements to optimal health—including after a COVID-19 infection and beyond.