You’ve had a busy day, and you plop into bed bone-tired. You get good sleep, and the next day carry on as normal. That’s what you expect, right? If you have chronic fatigue syndrome, things are much different. The next day, you wake up unrefreshed, as if you’ve gotten no sleep at all. You can barely get out of bed. When you stand up, you’re immediately lightheaded and nauseous. You have a headache you just can’t shake.
Life with chronic fatigue syndrome can often be unbearable. You want to be able to do the things you enjoy–and the things you have to do–but even brushing your teeth can feel like an insurmountable chore.
On top of that, many providers don’t understand chronic fatigue syndrome, sending those with the condition struggling to receive a diagnosis and bouncing around from treatment to treatment. Keep reading to learn more about chronic fatigue syndrome, how it's diagnosed, ways to manage symptoms, and how you can start to feel like yourself again.
Understanding chronic fatigue syndrome
Chronic fatigue syndrome (CFS) is also called myalgic encephalomyelitis (ME). “This is a serious, chronic multisystem illness that can often be disabling,” says Peter C. Rowe, MD, member of Solve M.E.’s Research Advisory Council (@solve_cfs) and director of the Children’s Center Chronic Fatigue Clinic at Johns Hopkins Medicine in Baltimore.
People with CFS may have such profound exhaustion not improved with rest, plus aches and pains and brain fog, that they’re no longer able to attend work or school or enjoy social events.
So what triggers this cascade of full-body exhaustion that you just can’t seem to shake? “Myalgic encephalomyelitis is often–but not always–triggered by factors like an infection, trauma, or surgery. However, we don’t fully understand how it develops,” says Dr. Rowe. What is clear is that even if the cause hasn’t yet been determined, your symptoms are very real. In addition, conducting deep dive testing to look for clues about what caused your CFS is important in optimizing your treatment plan.
Not sure what your symptoms are really telling you?
The Parsley Symptom Index helps connect the dots across your whole body so you can understand patterns, not just isolated symptoms.
Symptoms and diagnosis
Chronic fatigue can be a truly debilitating disease, reducing your ability to function and carry out daily tasks like showering, causing difficulty working or going to school, and impacting your ability to maintain a social life. Dr. Rowe points to diagnostic criteria for ME/CFS from the Institute of Medicine. All three of the below symptoms are required:
- A reduction in the ability to engage in activities (work, school, social) that’s accompanied by new, profound fatigue. This has lasted more than six months.
- Post-exertional malaise, which means symptoms worsen 12 to 48 hours after physical, mental, or emotional exertion. “You can have a busy day and a good night’s sleep but are not okay the next day. When you push through an activity, you pay for it,” says Dr. Rowe.
- Unrefreshing sleep that leaves you still tired even after a full night of sleep.
In addition, you need to have one of two of the following additional symptoms:
- Brain fog, such as problems with thinking, memory, executive functioning, or information processing that’s made worse with exertion.
- Orthostatic intolerance, which means symptoms like lightheadedness, fainting, fatigue, brain fog, headaches, and nausea worsen when standing up.
According to the Centers for Disease Control and Prevention, additional symptoms that may be present (but aren’t needed for a diagnosis) include:
- Allergies/sensitivities to foods, odors, chemicals, medications
- Chills/night sweats
- Joint pain
- Muscle pain
- Nausea
- New headaches
- Sensitivity to light and sound
- Sore throat
- Swollen lymph nodes in the neck or armpit
- Visual disturbances
CFS is often considered a diagnosis of exclusion. “When we have patients who say that they’re just so tired, they sleep all day and night but are living with headaches, joint pain, and forgetfulness, we start considering chronic fatigue syndrome, but there are a lot of other symptoms of other diseases that can mimic it,” says Vicky Bakhos Webb, MD, owner at Vie Concierge Family Medicine & Aesthetics in Midland, Texas.
Clinicians should run blood work to rule out additional causes of fatigue, such as anemia, thyroid dysfunction, or electrolyte imbalance. Clinicians may advise a sleep study to screen you for sleep apnea, says Dr. Webb.
Also remember that it’s possible to have more than one thing going on at once. Other disorders cause orthostatic symptoms like postural orthostatic tachycardia syndrome (POTS), which clinicians find frequently occurs alongside CFS. In addition, clinicians should consider mast cell activation syndrome (MCAS) as potentially co-occurring with CFS. MCAS can develop due to the gut bacteria disruption that occurred after an infection (the original CFS trigger). Some specialists consider MCAS a potentially overlooked and treatable contributor to CFS symptoms.
Treatment Plan
Here’s where things get truly tricky: According to the CDC, there is no cure or approved treatment for chronic fatigue syndrome. Another reality is that most people do not spontaneously get better–specific treatment is needed, says Dr. Rowe.
Personalized treatment is needed. The right treatment plan is tailored to each individual based on their unique health history, symptoms, and test results. There is no one-size-fits-all approach.
Treatments involve medication, symptom management, and lifestyle changes. The CDC recommends addressing the symptom that you find most life-disruptive first. Once you feel some improvement, you can move on to target another symptom.
One important goal, says Dr. Rowe, is to improve blood flow to the brain and support healthy circulation. This is often done with medication, but that can be complex. “It’s tricky to find the right treatment for each person because it won’t be the same medication,” he says. For example, for symptoms that occur with standing (orthostatic intolerance), providers may consider stimulants like methylphenidate (Ritalin), orthostatic drugs like midodrine, or beta-blockers like atenolol to control a racing heart rate, says Dr. Rowe.
Medications may also be used to treat specific symptoms, like headaches, which can make your day-to-day life better. For fibromyalgia-like aches and pains, pregabalin (Lyrica) may be prescribed, says Dr. Rowe. Headaches may benefit from supplements like vitamin B2 (riboflavin) or a prescription for a preventative migraine medication.
In addition, antidepressant medications like SSRIs may also help manage both the emotional toll of the condition and may also aid in fatigue, adds Dr. Webb. Talk to your provider about your specific symptoms and if there is a medication option that may be right for you. That said, medication is not the only tool needed in recovery.
In addition to medication as needed and appropriate, your clinician may also consider the following types of treatments based on the underlying contributors to CFS and test results:
- Addressing hormonal imbalances, particularly in the HPA (hypothalamic-pituitary-adrenal) axis.
- Detoxification, especially if toxin exposure is identified as a contributing factor.
- Gut health, including healing leaky gut, balancing the gut microbiome, and addressing any gut infections.
- Mitochondrial support to improve mitochondrial function and energy production at the cellular level.
- Treating co-infections if viral, bacterial, or fungal infections are identified as contributing factors.
Lifestyle changes for recovery
Lifestyle changes are hugely important to getting you to a place where you feel as if you can go out into the world again and start doing the things you have and love to do.
Dietary changes, sleep hygiene practices, stress reduction techniques, and carefully graded exercise programs are all recommended. Here’s a closer look at some of the important lifestyle changes:
Activity management
Activity management involves a slow and steady increase in regular activity with the goal of building up your physical tolerance without triggering post-exertional malaise. Dr. Rowe recalls a young woman who, after improving her functionality with two medications, began to ride a recumbent exercise bike for two minutes a day, increasing her time on that bike by one minute a week. “By two or three months, she was biking 30 minutes every day, and she was able to reduce her medication,” he says.
Nutritional support
When it comes to what you eat, Dr. Webb recommends limiting added sugar to avoid energy crashes. Also, if lab testing shows that you’re deficient in nutrients (such as iron)talk to your clinician about taking a supplement. Addressing nutrient deficiencies through diet and supplementation is often a core part of treatment. This may include vitamins, minerals, antioxidants, and other targeted nutrients.
Sleep hygiene
Although you know that “sleeping more” isn’t the answer, setting yourself up for good sleep is another strategy Dr. Webb recommends. That means maintaining a regular sleep schedule, setting up your room to be cool, dark, and quiet, and avoiding electronic devices before bed. Those things were important before, but are even more important when you have a condition like CFS that causes fatigue.
Mind-body techniques
Having CFS is stressful and it can greatly affect your mood and mental health. Practices like meditation, yoga, and cognitive behavioral therapy (more on that below) may be incorporated to address the psychological aspects of CFS.
Healing stories from our members
Coping mechanisms
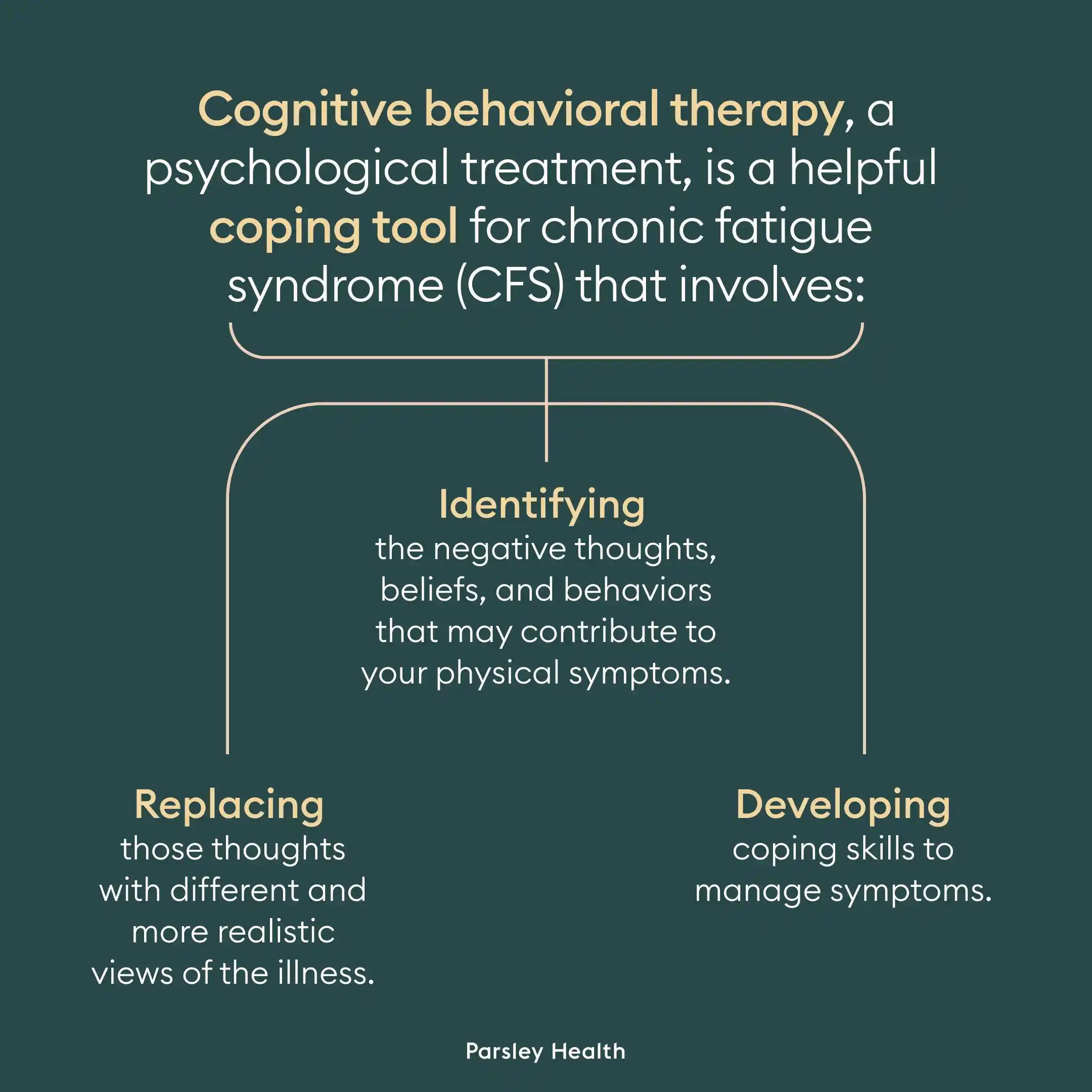
Cognitive behavioral therapy, or CBT, is frequently recommended as a treatment strategy, and one that may be a helpful coping tool, says Dr. Webb. CBT is a psychological treatment that involves:
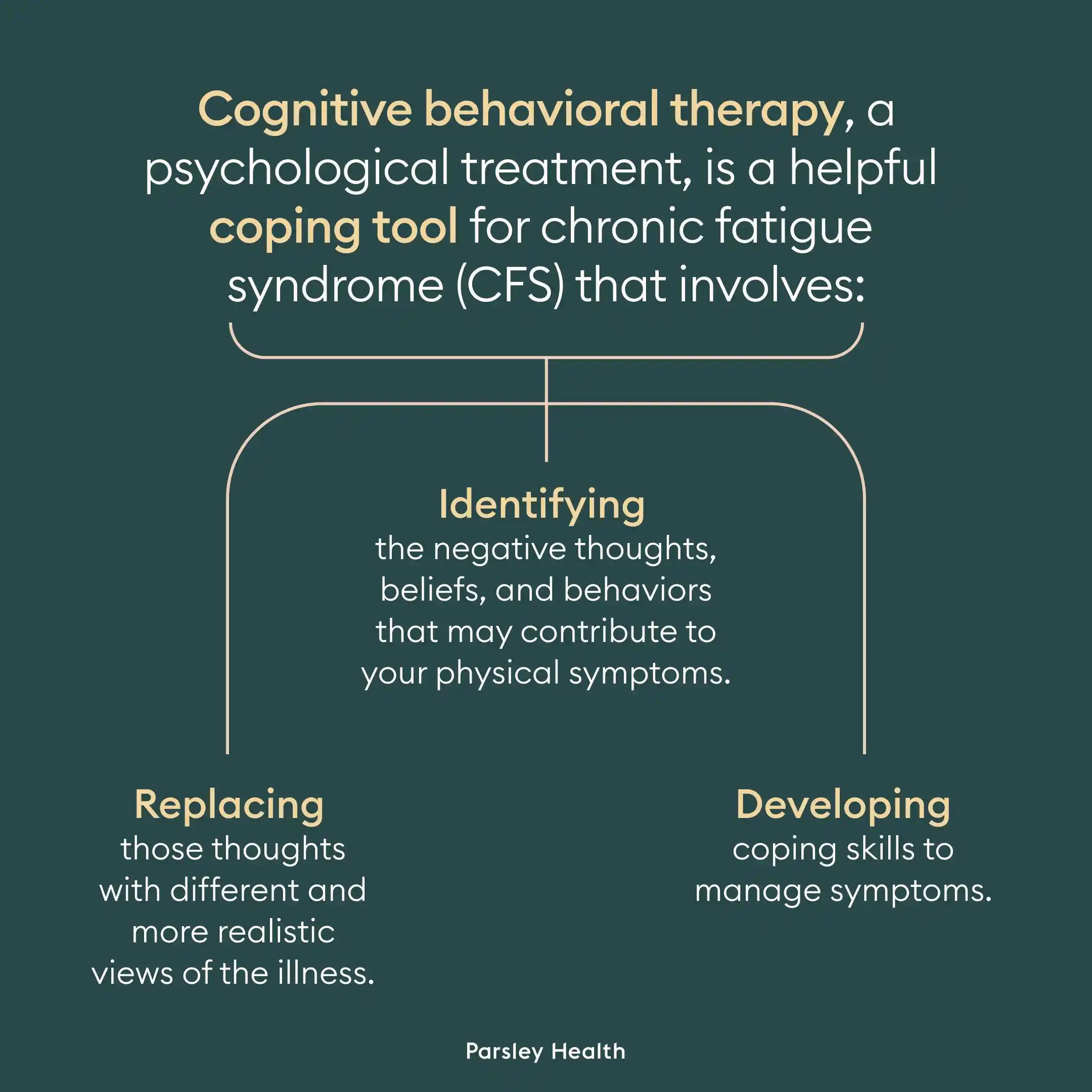
- Identifying the negative thoughts, beliefs, and behaviors that may contribute to your physical symptoms.
- Replacing those thoughts with different and more realistic views of the illness.
- Developing coping skills to manage symptoms.
CBT addresses the two goals of treatment, which is to increase activity levels and improve physical functioning. A recent meta-analysis spanning 15 randomized controlled trials and over 2,000 people, CBT was more effective for relieving fatigue, depression, anxiety and improving health compared to controls, with treatment ranging from 8 to 36 weeks. What’s more, people found it relatively easy to stick to a CBT practice.
One of the studies in that meta-analysis was a trial published in Frontiers in Psychiatry on 236 patients with chronic fatigue syndrome. Those with mild to moderate disease who received CBT for 16 weeks benefited from improved physical function and fatigue. Half of the CBT group improved their physical functioning score compared to 20 percent in the control group. CBT also helped improve mental health, pain, social functioning, and vitality. The authors of this study are quick to point out that just because CBT may have a positive impact on symptoms, it doesn’t mean that CFS is a psychological condition.
Although CBT can provide useful and impactful coping skills for some, CBT is not curative. “It can be helpful for patients who have trouble cognitively, but it’s not helpful for everyone,” adds Dr. Rowe.
Overcoming setbacks and relapses
Recovery from CFS is often a gradual process. Functional medicine emphasizes ongoing support and adjustments to your treatment plan when needed.
As such, it’s hard to provide a timeline on when you’ll start feeling better or when you’ll be able to get through a work day again. CFS may be something you’ll have to learn to live with for a long time, says Dr. Webb. That’s not discouraging at all–knowing that can help you approach setbacks and relapses with the knowledge that this is normal and you’re still moving forward and making progress.
One common cause of a crash is overextending yourself on a good day, says the CDC. When you’ve felt extreme fatigue for so long and finally gather some energy, you may be tempted to try to do too much, which is too taxing on your body. It’s normal to feel discouraged, but you can use this as a learning opportunity–your body is telling you where your boundaries are. That’s great information to have. You can use this information to help you honor your body’s needs to avoid these crashes in the future. Eventually–and slowly–you can get back to a place where you do it all again–many people have found it to be possible.
My recovery journey
Rebecca Tolin spent 13 years living with chronic fatigue syndrome and chasing various solutions via a variety of specialists before she tried mind-body healing. This treatment focused on three things: retraining her brain, regulating her nervous system, and working with her emotions. For example, she would challenge herself to walk around the block. When symptoms arose (as expected), she’d remind herself that these were warning signals from her body, but she was not in actual danger or harming herself–it was her nervous system overreacting. “I’d come home from a walk and do somatic tracking, which involved focusing on the sensations in my body. I’d tell myself I was safe and okay. I used guided meditations to help me through this process,” she says.
Her full recovery journey took nearly a year, but she was able to go back to working full time, socializing, and exercising regularly. Now, 54, the San Diego, California life coach and mind-body practitioner “feels fantastic,” she says. “I have great energy. I feel calm and safe in my body. I live a really full life.”
Liz Carlson, 38 (@healwithlizc), caught a flu-like virus shortly after her 30th birthday and wasn’t able to recover. She, too, struggled to get a diagnosis and find the right treatment, trying a variety of remedies, none of which helped her fully recover. Until she started using a brain retraining program: “I spent one hour each day visualizing myself thriving. This wasn’t positive thinking, it was trying to get to my body by using my mind,” she says. It’s something that she says helped her nervous system come down from high alert. “I fully slept through the night after my first session,” she says. As she started feeling better, she was able to increase her activity, eventually walking two miles or swimming 1,000 meters in the pool.
By 2019, the Orinda, California resident and CFS advocate had mostly recovered, she says. One of her favorite visualizations was imagining herself paddleboarding, something she did on her honeymoon that year. Still, the consequences of the illness are still fresh in her mind. “I lost three years where I was in the prime of my life,” she says.
Mind-body therapies encapsulate a variety of treatments, such as relaxation, movement-based therapy (certain forms of yoga, Qigong), and mindfulness and cognitive-behavioral approaches. One review notes that these may work due to neuroplasticity–or the ability of our brains to form new neural connections. If you can retrain your brain to process your thoughts, feelings, and emotions surrounding physical symptoms, you can feel less distressed by them. And while this review concluded that research has shown an improvement in fatigue, functioning, and anxiety and depression compared to controls, more studies are needed. What’s more, mind-body practices may not be right for everyone.
When to seek medical help
To be diagnosed with chronic fatigue syndrome, clinicians consider if you’ve had symptoms for at least six months. That is a long time to exist with crushing fatigue–do not wait that long to seek help, says Dr. Webb. See your doctor if you’re experiencing symptoms of post-exertional malaise where physical or mental activity causes extreme fatigue that worsens over the next one to two days. (This is exhaustion that does not make sense with the amount of activity you just did, such as showering or doing a load of laundry–not, say, running a half marathon.)
If standing or sitting upright feels terrible due to dizziness, a racing heart, or weakness, you should also talk to a provider, as these are signs of orthostatic intolerance, another hallmark symptom of the condition.
Debilitating fatigue may be caused by CFS, but there may also be other causes, such as anemia or thyroid dysfunction, which you should be tested for and addressed, if needed.
It’s so important to find a good support system. “You need people who do not take your condition lightly or brush it off,” says Dr. Webb. “When patients get the support they need from providers and family members, they start doing better,” she says.
Parsley Health offers physician-led functional medicine care, advanced lab programs, and flexible ways to get started, all designed to help you feel better over time.
Frequently asked questions (FAQs)
How to reverse chronic fatigue?
Although there is no single cure for chronic fatigue, there are a number of tools that can help you get back to living a full life. Those include medications, symptom management, and lifestyle changes like activity pacing and proper sleep habits. CFS is treated holistically and with a customized combination of treatments.
How to get more energy when you have chronic fatigue?
One of the best things you can do is to increase your activity tolerance with exercise. This means starting with very small amounts of movement and gradually, slowly building up from there.
Can you push through chronic fatigue?
Do not try to push through chronic fatigue as that can worsen symptoms of fatigue. You can make small changes to routine activities in order to better tolerate them, such as taking frequent breaks while doing tasks. However, pushing yourself past your physical limits can bring on a crash, or a rebound of symptoms.
How do you live with constant fatigue?
This can be a real challenge. Taking breaks, making daily tasks easier on yourself (and letting things go or asking others to do them) can help you get through your day. In addition, using the technique of activity management, whereby you very slowly increase exercise can also help. In addition, taking care of your mental health through counseling and/or medication can help address the emotional component of this condition.
How to help someone with chronic fatigue?
One of the best things you can do is to respect what they’re going through. Even if they seemed perfectly healthy before, their extreme fatigue now is real and it’s debilitating. They need someone in their corner who can offer support and help if needed. Can you take over a task for them like grabbing groceries or pre-made healthy meals next time you’re at the store? Can you offer to walk down the block and back with them? Or can you listen to them if they express frustration with their symptoms?
Chronic fatigue syndrome/myalgic encephalomyelitis is a condition where you experience extreme exhaustion with normal activity despite adequate rest. It can also bring about joint pain, brain fog, lightheadedness/dizziness when upright, and depression and anxiety. Although researchers are still unsure about the exact causes, CFS is not “all in your head”--this is a very real, physical illness.
After a diagnosis, what’s most important is using therapies that address your symptoms, which can include medical management, lifestyle changes, and coping strategies. The journey to recovery can be tough, there’s no doubt about that, but you can take it with a compassionate clinician who caters your care to your needs like a clinician with Parsley Health.