This article contains additional reporting by Angela Myers.
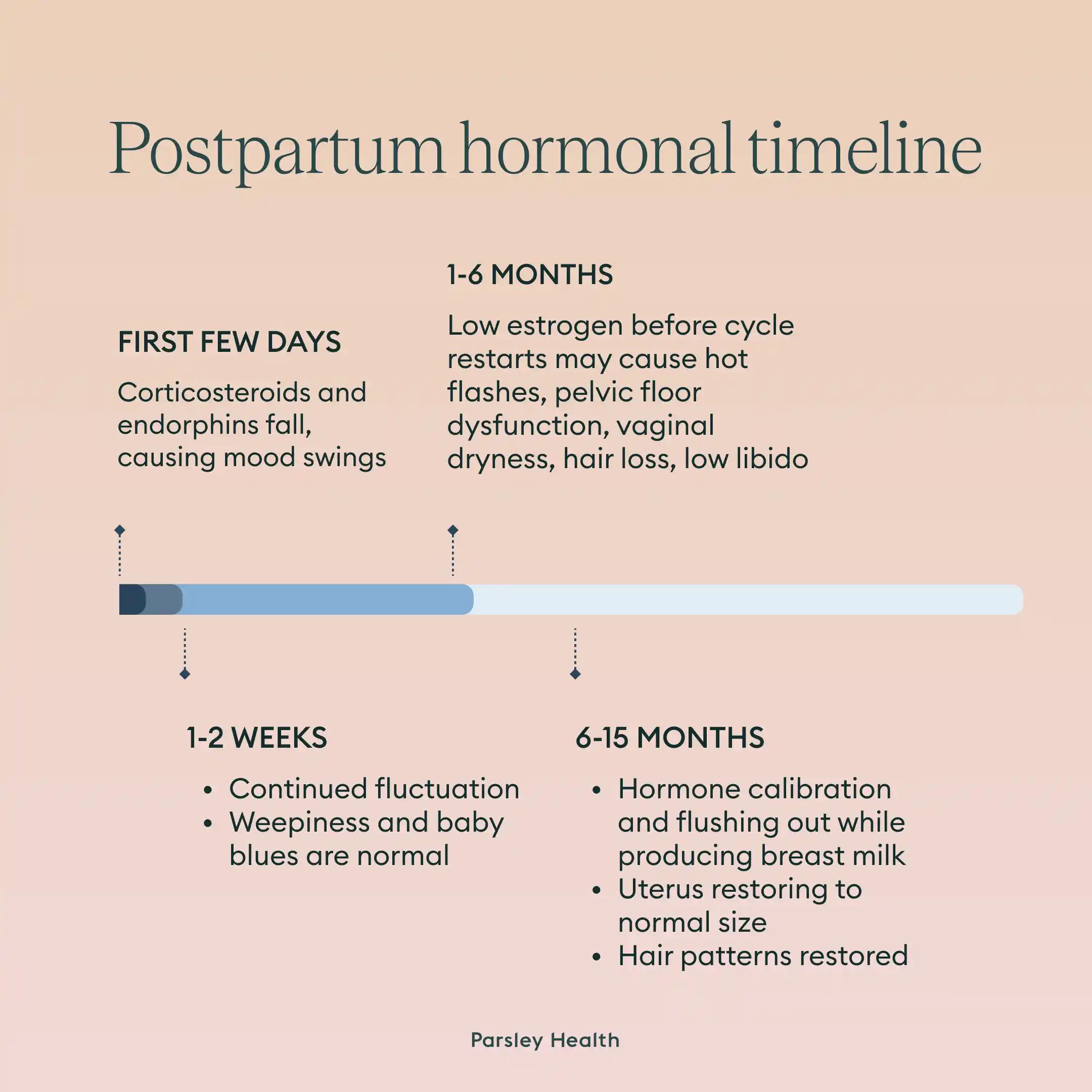
Almost everyone who gives birth experiences postpartum hormone fluctuations and while it’s new, it’s normal. That said, you should know what’s happening in your body and why, so we talked to two Parsley Health experts about what to expect from your hormones after you give birth, how long these changes will last, and signs of hormone imbalance after pregnancy.
Signs of a Hormone Imbalance After Pregnancy
If you’ve recently given birth, your body is going through natural hormonal fluctuations that might make you feel a little different (on top of, you know, having a baby.).
Postpartum hormonal imbalance symptoms can include:
- Mood swings
- Fatigue
- Low or non-existent sex drive
- Irregular menstrual cycles
Mood Swings
We've all heard of postpartum depression, a condition where a mother feels depressed after giving birth due to hormonal fluctuations. Postpartum depression is diagnosed in one in six new moms. Diagnosis or not, you can still experience mood swings, the baby blues, or anxiety after giving birth.
Fatigue
Exhaustion is a constant companion for parents, especially when postpartum. If feeling fatigued, sleep can do wonders, but for obvious reasons, it’s the most challenging to prioritize. Taking naps when you can and enlisting childcare support from friends, family members or childcare providers. These drug-free ways to get better sleep may also be helpful.
Low or Non-existent Sex Drive
Breastfeeding hormones can lower a new mother's sex drive and may even cause vaginal dryness and pain during sex. Usually, hormones and your sex drive return to normal once you're done breastfeeding.
Irregular Menstrual Cycles
Having an irregular period is normal after giving birth. For many new mothers, it can take months to get back to a normal flow, and even longer if you continue to breastfeed past the six month mark.
Weight Gain
Gaining weight while pregnant is normal. Usually, half that weight disappears six weeks after childbirth and the rest comes off over the next few months.
Christina Kang, a former health coach at Parsley Health encourages patients to avoid worrying about weight loss for the first 3 to 6 months after giving birth. “With patience, good nutrition, and moderate exercise, much of the weight will come off on its own over a period of time. When people are overly restrictive, the body may hold on to excess weight in order to have enough fuel to continue making breast milk,” she says.